How to Identify Food Sensitivities a Practical Guide

Figuring out your food sensitivities is really a three-part investigation: you observe, you eliminate, and then you reintroduce. It’s a process of self-discovery that helps you draw a straight line from symptoms like bloating or brain fog to the specific foods causing them. No more guesswork, just clear answers.
Decoding Your Body's Subtle Signals
Ever wonder why you feel bloated after a seemingly healthy lunch, hit a wall of fatigue mid-afternoon, or can't seem to shake a skin issue? The answer is often hiding right on your plate. A food sensitivity is your body's unique, non-allergic negative reaction to a certain food, and its signals can be frustratingly subtle and delayed.
This is very different from a food allergy, which triggers an immediate and sometimes severe immune response. It's also not the same as a food intolerance, which usually comes down to a missing digestive enzyme (like in lactose intolerance). Getting a handle on the difference between food intolerance and allergy is key, because sensitivities are far more nuanced. Reactions can pop up hours or even a few days after you’ve eaten the trigger food.
Connecting Symptoms to Your Plate
Let’s get practical. A single meal can set off a chain reaction of what feel like totally unrelated symptoms. That morning brain fog you're blaming on a bad night's sleep? It could actually be the gluten in your toast. That stubborn eczema on your hands might be linked to the dairy in your daily latte. These connections are deeply personal and easy to miss without a structured approach.
Some of the most common signs of a food sensitivity include:
- Digestive Upset: Bloating, gas, constipation, or diarrhea.
- Brain & Energy Issues: Brain fog, trouble focusing, or just feeling drained.
- Skin Problems: Eczema, acne, mysterious rashes, or hives.
- Mood Swings: Irritability, anxiety, or a dip in your mood.
- Aches and Pains: Headaches, migraines, or joint pain.
Spotting these patterns is the first real step toward feeling better. You have to become a detective for your own body, gathering clues from your daily life.
The bottom line: A food sensitivity isn't a dramatic, immediate reaction like an allergy. It’s more of a low-grade, chronic response that can quietly chip away at your health over time. Learning to read your body’s unique language is crucial.
You're not alone in this. Adverse food reactions are incredibly common worldwide. While true food allergies get a lot of attention, sensitivities are far more widespread. In fact, self-reported negative reactions to food range from 3% to 35% across 51 global studies. That huge range shows just how many people are struggling to connect what they eat with how they feel, often without a clear path forward.
To help with that, I’ve broken down the entire process into a clear, manageable plan. This table gives you a bird's-eye view of the journey we’re about to take.
Your Roadmap to Pinpointing Food Triggers
This simple, three-phase process is your key to finally getting some answers.
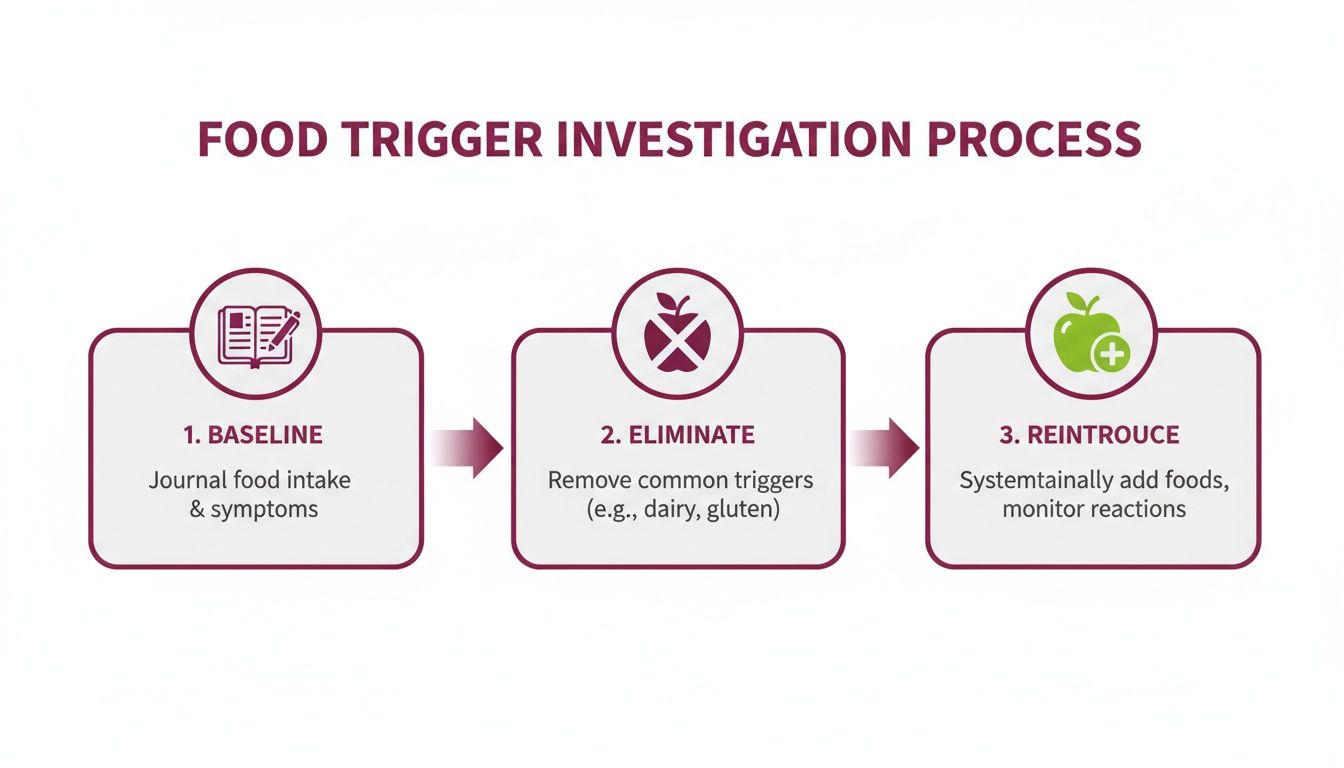
Each step—establishing your baseline, carefully eliminating the suspects, and then methodically reintroducing them—is designed to build on the last. By following this structure, you can move from confusion and frustration to clarity and control over your health.
Getting to Know Your “Normal” Before You Change a Thing
Thinking about jumping straight into an elimination diet? Hold that thought. It’s a bit like trying to navigate a new city without a map. Before you cut out a single food, the most important first step is to simply observe. This is all about creating a detailed snapshot of your current reality—your personal health baseline.
For two full weeks, you’re a detective on a case. Your only job is to pay close attention and record your findings without changing your diet or judging what you see. This period gives you the crucial "before" picture. Without it, you’ll have no real way to measure the "after" and know for sure if your dietary changes are making a difference.
What to Track for a Clear Picture
Good tracking is way more than just jotting down what you ate for lunch. You're aiming for a complete view of your day, connecting what you consume with how you feel, both physically and mentally. A vague note like "felt tired" won't help you much later on. The more detail you can capture, the easier it will be to spot the patterns.
Here’s what your daily log should cover:
- Food and Drink: Get specific with everything you consume. List meals, snacks, drinks, condiments, and even supplements. Instead of just "salad," write down "spinach, grilled chicken, tomatoes, feta cheese, balsamic vinaigrette." Brands can matter, too!
- Symptom Details: Note any physical or mental symptoms. How severe was it on a scale of 1-10? When did it start? How long did it last? This could be anything from a dull headache hitting at 3 PM to sharp stomach cramps right after dinner.
- Energy Levels: How’s your energy from morning to night? Did you wake up refreshed or drag yourself out of bed? Did that classic mid-afternoon slump hit you hard? Note specific times you felt energized versus wiped out.
- Mood and Mind: Your emotional state is a huge piece of the puzzle. Log feelings like irritability, anxiety, or brain fog. On the flip side, note moments of unusual clarity or focus. Since stress can often make sensitivities worse, tracking your stress levels is also a game-changer.
You're not just keeping a food diary; you're building a personal health database. This data is the very foundation of your entire investigation.

Modern tools can make this process feel less like a chore. For example, an app like Superbloom can help you log symptoms and meals in the moment and even uses AI to help you spot connections you might have missed on your own.
How to Make Baseline Tracking Stick
Consistency is absolutely key during these two weeks. The best way to stay on track is to find a method that actually fits into your life.
Whether you're a pen-and-paper person with a dedicated notebook, prefer a notes app on your phone, or want to use a specialized tool, just pick one and stick with it. My pro tip? Set a recurring reminder on your phone for right after each meal to log everything while it’s still fresh in your mind.
Let's look at what a really solid entry looks like in practice:
This is the level of detail you’re shooting for. After two weeks of this kind of focused observation, you'll have an invaluable collection of personal data. You might even start noticing some potential culprits on your own. This baseline isn’t just a step to get through—it’s the most critical part of the entire process.
Navigating The Elimination Phase With Confidence
Alright, you’ve got your baseline data. Now comes the part where the real detective work begins: the elimination phase. This is the most powerful step in figuring out what’s really going on with your body. The goal here is simple but crucial: you’re temporarily removing the most common trigger foods to give your system a much-needed break. Think of it as hitting the reset button on your body's inflammation, which allows it to send much clearer signals later on.

This process usually lasts for about three to four weeks. I know that can sound like a long time, but sticking to it is essential. It gives your body enough time for any lingering inflammation to calm down and for your system to fully adjust. The key to success here is a mental shift—stop focusing on what you're taking out and start getting excited about all the delicious, nourishing foods you can still enjoy.
Choosing What To Eliminate
While there are over 160 different foods that have been known to cause a reaction, you absolutely do not need to cut them all out. That would be miserable and totally unnecessary. The smartest approach is to start with the "usual suspects"—the handful of foods that account for the vast majority of sensitivities.
For most people I work with, this is the most effective starting list:
- Gluten: Found in wheat, barley, rye, and lurking in tons of processed foods.
- Dairy: This includes milk, cheese, yogurt, and butter.
- Soy: Obvious sources are tofu and soy milk, but it's often a hidden ingredient.
- Corn: Found everywhere from fresh corn to corn syrup and cornstarch.
- Eggs: A common trigger, whether in baked goods or on their own.
- Refined Sugar & Artificial Sweeteners: These can fuel inflammation and disrupt gut health.
This targeted strategy is far more practical than a scorched-earth approach. It's about being strategic, not restrictive for the sake of it. In fact, while some questionnaires might suggest sensitivities are widespread, more rigorous testing shows that up to 15-20% of adults experience real IBS-like symptoms from them. Since the top 8 allergens (including milk, eggs, and peanuts) cause 90% of reactions, focusing on this small group first is the most efficient way to get answers.
Master The Art Of Reading Food Labels
During this phase, you’ll need to become a bit of a food detective. Food labels are your new best friend. Trigger ingredients love to hide under strange-sounding names, so just glancing at the front of a package won't cut it. You have to get in the habit of flipping that box over and reading the entire ingredient list, every single time.
For instance, "casein" or "whey" on a label means it contains dairy. Gluten can pop up in soy sauce or even salad dressings. This is why scrutinizing labels and understanding every ingredient, including common additives like bulking agents in food, is so important. Your diligence here is what ensures you're actually creating that "clean slate" your body needs to communicate with you.
Key Takeaway: See this phase as an empowering reset, not a punishment. Every meal is an opportunity to be kind to your body, giving it the space it needs to heal and finally tell you what it needs.
Focus On Abundance, Not Restriction
Here's the secret to not just surviving, but thriving during elimination: focus on what you get to eat. Your plate should be overflowing with vibrant, delicious, and nutrient-packed foods. This is about discovery, not deprivation.
This is your chance to lean into foods like:
- Lean Proteins: Chicken, fish, turkey, grass-fed beef.
- Colorful Veggies: Pile on the leafy greens, broccoli, sweet potatoes, bell peppers, and zucchini.
- Healthy Fats: Avocado, olive oil, coconut oil, and (if they aren't on your elimination list) nuts and seeds.
- Gluten-Free Grains: Quinoa, rice, buckwheat, and certified gluten-free oats are all great.
- Flavorful Herbs & Spices: These will be your secret weapon for making every meal incredible.
To make things even easier, here’s a quick-reference table for some simple food swaps.
Common Food Triggers and Simple Swaps
Navigating the grocery store can feel a bit tricky at first, but with a few simple swaps, you won't feel like you're missing out. This table is a go-to guide for common foods to avoid during elimination and some easy, tasty alternatives to keep your meals interesting and satisfying.
Having these alternatives in your back pocket makes meal planning and cooking much less intimidating. It's all about finding new favorites.
Meal prepping is an absolute game-changer here. I recommend spending a couple of hours on the weekend roasting a big batch of vegetables, cooking some quinoa, and grilling chicken or fish. Having these building blocks ready to go makes it incredibly easy to assemble a compliant, delicious meal during a hectic week. Honestly, preparation is your best defense against feeling overwhelmed and grabbing something you'll regret later.
The Reintroduction Phase: Listening to Your Body
After several weeks of clean eating, your body is in a much calmer, less inflamed state. This is the moment you’ve been working toward. The reintroduction phase is where the real lightbulb moments happen, turning your vague suspicions into clear, undeniable answers.
This isn’t about jumping right back into your old habits. Think of it as a slow, methodical experiment where you are both the scientist and the test subject. The goal is simple: reintroduce one food group at a time, very carefully, and listen intently to what your body tells you.
The Art of the Single Food Challenge
The absolute golden rule of this phase is isolation. You must test only one potential trigger food at a time to get an accurate read. If you bring back gluten and dairy on the same day and feel awful, you’re right back where you started—unsure which one was the real culprit.
Here’s a simple, effective protocol I've seen work time and again:
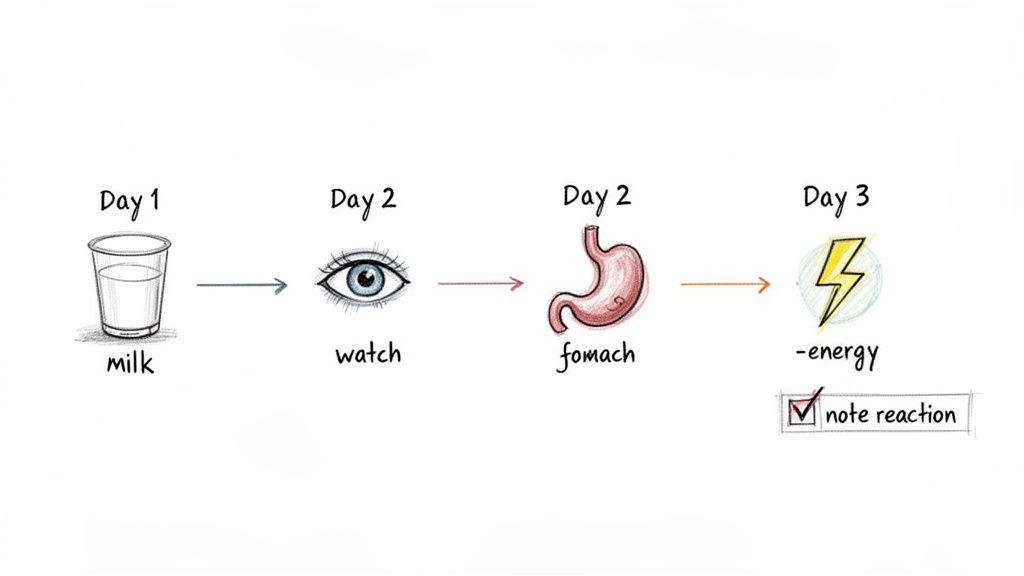
- Pick One Food: Choose a single food from your elimination list to test. Let’s say you start with dairy.
- Eat It Intentionally: On your reintroduction day (let's call it Day 1), have a normal serving of that food two or three times. For example, a glass of milk in the morning and some cheese with your lunch.
- Wait and Watch: For the next two to three days (Day 2 and Day 3), don't introduce anything else. Go straight back to your clean, elimination-style diet and just pay attention.
- Record Everything: This is crucial. Meticulously log any and all symptoms that pop up during this observation window. Did you feel bloated? Did a headache creep in? Was your sleep off?
This patient, three-day cycle for each food is non-negotiable. While some reactions are immediate, many are delayed and can take up to 72 hours to fully show up. Rushing the process is the single biggest mistake people make, and it completely undermines all the hard work you’ve put in.
Interpreting Your Body's Feedback
Your body communicates through symptoms. During reintroduction, your job is to become a fluent interpreter. Sometimes the feedback is loud and clear, like immediate bloating after eating a piece of bread. Other times, it’s much more subtle—a slight increase in joint stiffness the next morning or finding yourself in an irritable mood for no apparent reason.
Keep an eye out for these common signals:
- Digestive Upset: Gas, bloating, stomach cramps, diarrhea, or constipation.
- Head and Mood: Headaches, migraines, brain fog, irritability, or anxiety.
- Skin Reactions: Rashes, hives, eczema flare-ups, or acne breakouts.
- Energy and Sleep: A sudden crash in energy, trouble falling asleep, or waking up feeling like you barely slept.
Let’s walk through a real-world scenario. On Monday, you reintroduce eggs. You have two for breakfast and feel totally fine. On Tuesday, you go back to your usual elimination diet, but you notice you’re unusually tired in the afternoon and a dull headache starts that evening. By Wednesday morning, a couple of pimples have appeared on your chin. Those are classic delayed signals of a sensitivity.
By carefully logging your experience with each food group, you finally get the concrete answers you've been looking for. This isn't guesswork; it's a systematic experiment where you gather direct, personal data.
The rise in food sensitivities seems to mirror modern life. That’s why consistent symptom-food mapping during this phase is so important, especially when you consider that for adults, over 50% of new-onset allergies appear after age 18. Recognizing these patterns—a process made much easier with journaling tools like the Superbloom app—is what lets you pinpoint your personal triggers and take targeted action, instead of just restricting your diet unnecessarily. You can find more on these recent findings in food reaction studies.
Making Long-Term Decisions from Your Results
Once you've tested a food and gathered your notes, you have a choice to make.
If a food caused a clear, negative reaction, the answer is straightforward: keep it out of your diet for now. This doesn't have to be forever. You can always try retesting it again in a few months, as our sensitivities can sometimes change over time.
If a food caused no reaction at all, congratulations! You can safely welcome it back into your regular eating rotation. Just take a day to eat clean again to reset your system, and then you're ready to test the next food on your list.
This careful, step-by-step process is the most reliable way to identify food sensitivities because it’s based entirely on your own unique biology. It moves you from a life of confusing symptoms to a future of vibrant health and clarity, empowering you to build a personalized diet that truly makes you feel your best.
When to Bring in the Pros
Going through an elimination diet on your own can be incredibly empowering. You’re learning to listen to your body and connect the dots between what you eat and how you feel. It’s a powerful process.
But this DIY approach isn't always the full picture. Knowing when to call in a healthcare professional is just as crucial as knowing how to track your symptoms. It isn’t a sign you’ve failed; it’s a smart, responsible step toward getting the right answers and ensuring your long-term health.
Sometimes, the signals your body is sending are too confusing—or too severe—to navigate alone. There are a few clear red flags that mean it's time to pause your own investigation and get guidance from a doctor, registered dietitian, or allergist.
Clear Signs You Need Professional Help
Self-managing your diet is fantastic for uncovering sensitivities, but it can't replace a real medical diagnosis, especially when something more serious might be going on. If you experience any of the following, it’s time to make an appointment.
- Immediate or Severe Reactions: If you reintroduce a food and immediately get hives, swelling, wheezing, or have trouble breathing, stop. This is not a sensitivity. These are the hallmarks of a true IgE-mediated food allergy, which can be life-threatening and demands immediate medical attention.
- You Suspect Celiac Disease: If gluten gives you a seriously bad reaction, don’t just write it off as a sensitivity. A doctor needs to properly test for Celiac disease—an autoimmune disorder—before you cut out gluten. The standard tests only work if you’re still actively eating it.
- Your Symptoms Just Won't Quit: You’ve done the work. You’ve gone through the entire elimination and reintroduction process, but your digestive upset, skin rashes, or crushing fatigue are still there. This might point to something more complex that an elimination diet can't fix, like SIBO (Small Intestinal Bacterial Overgrowth) or another underlying gut condition.
- You're Worried About Nutrition: If your list of "no" foods is getting alarmingly long, you're at risk for nutritional gaps. A registered dietitian is the perfect partner here. They can help you craft a safe, balanced, and enjoyable way of eating that doesn’t leave you missing key nutrients.
Being your own best health advocate means knowing your limits. That food-and-symptom journal you’ve been keeping? It’s pure gold. Bring it with you. It makes the conversation with a professional instantly more productive.
It transforms a vague complaint like "I always feel tired" into a concrete observation: "I feel exhausted and foggy-headed within 3 hours of eating anything with wheat."
Understanding the Professional Testing Options
Once you do see a professional, they have a whole toolkit of diagnostic tests they can use. It's helpful to know the difference between validated medical tests and some of the others out there that don't have strong scientific backing. This is a key part of learning how to identify food sensitivities with expert support.
Your healthcare provider might suggest a few things:
- IgE Allergy Testing: This is the gold standard for identifying true food allergies. It’s usually done with a skin prick test or a blood test that measures Immunoglobulin E (IgE) antibodies—the specific kind that trigger allergic reactions.
- Celiac Disease Screening: This starts with specific blood tests that look for certain antibodies and genetic markers. A positive result is typically confirmed with an intestinal biopsy to check for damage.
- Breath Tests: These are really useful for diagnosing issues like lactose intolerance or SIBO. They work by measuring the gases your gut bacteria produce after you drink a specific sugar solution.
One word of caution: be wary of the widely available IgG food sensitivity tests you see online. Most medical organizations and practitioners don't consider these reliable for diagnosing sensitivities. An elevated IgG level often just means you’ve been exposed to a food, not that you have a problem with it. This can lead people down a rabbit hole of overly restrictive and unnecessary diets.
Working with a professional doesn’t mean your own detective work was for nothing—it actually makes it stronger. They can take the insights you've gained, place them in a broader medical context, rule out more serious conditions, and guide you forward. This collaborative approach is your surest path to feeling better for good.
Got Questions About Food Sensitivities? You're Not Alone.
When you first start digging into food sensitivities, a lot of questions pop up. It’s a pretty involved process, so it's completely normal to wonder about timelines, different testing methods, and even how to handle the emotional ups and downs. Let's walk through some of the most common questions I hear, so you can feel more confident moving forward.
How Long Until I See Results from an Elimination Diet?
This is usually the first thing people ask, and it’s a two-part answer.
You’ll probably start to feel some initial improvements within the first one to two weeks of cutting out certain foods. Many people report a noticeable boost in energy, less bloating, or a bit of that brain fog lifting pretty quickly.
But for those more stubborn, chronic symptoms—think skin issues like eczema or that nagging joint pain—it can often take the full three to four weeks for your body's background level of inflammation to really settle down. The key here is patience. The real "aha!" moments don't usually happen during the elimination phase itself; they come when you start reintroducing foods. That's when a reaction can show up, sometimes within a few hours, but sometimes not for a day or two.
The Difference Between a Food Sensitivity Test and an Elimination Diet
It's so easy to get these two mixed up, especially with all the at-home tests advertised online. Here’s the simplest way to think about it: a well-structured elimination and reintroduction diet is your body's own "gold standard" test. It gives you direct, undeniable feedback on how a specific food actually makes you feel in the real world.
On the other hand, many popular at-home food sensitivity tests, especially the ones that measure IgG antibodies, are not considered scientifically reliable by most doctors for pinpointing sensitivities. The big problem is that they often produce a ton of false positives. They might just be flagging a food you've eaten recently, not one that's actually causing a problem. This can lead people down a rabbit hole of overly restrictive and unnecessary diets.
It's important to know that this is completely different from a true food allergy test ordered by a doctor, which measures IgE antibodies and is a valid medical tool for identifying immediate, and often severe, immune reactions.
An elimination diet is the most accurate way to identify food sensitivities because it's based on your direct experience, not a lab report that may or may not reflect your reality.
I Feel Overwhelmed. Where Should I Start?
If you're looking at the whole process and it just feels like too much, you're in good company. My best advice? Take a deep breath and start with the simplest, most powerful first step: just observe. Don't even think about cutting anything out yet.
For the next one to two weeks, just commit to tracking what you eat and how you feel, exactly like we talked about earlier. Grab a simple notebook or use an app you like. This one small act of building awareness is the foundation for everything that follows. You'll likely be amazed at the patterns you uncover just by paying close attention, and that insight will give you the confidence to take the next step when you're ready.
Can Stress Make My Food Sensitivities Worse?
Yes, 100%. This connection is huge, and it’s something people often miss. Stress has a direct, powerful impact on your gut. It can increase intestinal permeability (you might have heard the term "leaky gut"), which in turn can make your entire system more reactive to the foods you eat.
Ever notice how you can eat a certain food while you're relaxed on vacation and feel totally fine, but that exact same meal gives you bloating or a headache during a high-stress week at work? That's the connection in action. This is precisely why tracking your mood and stress levels right alongside your food and symptoms is so important. Recognizing this pattern is a game-changer for managing your symptoms long-term, because it teaches you that feeling better isn't always about the food—it's also about managing your body's overall state of stress.
Ready to turn your observations into lasting change? The Superbloom app is designed to help you do just that. It uses AI-powered coaching to help you spot patterns between your food, mood, and symptoms without the stress of calorie counting. Start building healthier habits that stick by trying Superbloom today.